Late phase allergic
reactions may begin several hours after exposure to antigen. It is thought
that basophils play a major role here. Cell-bound IgE on the surface of
basophils of sensitive individuals binds a substance called histamine
releasing factor (possibly produced by macrophages and B-lymphocytes)
causing further histamine release.
The inflammatory agents
released or produced cause the following:
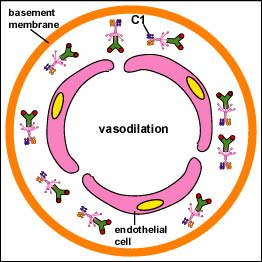
a. dilation
of blood vessels. This causes local redness (erythema) at the
site of allergen delivery. If dilation is widespread, this can contribute
to decreased vascular resistance, a drop in blood pressure, and
shock .
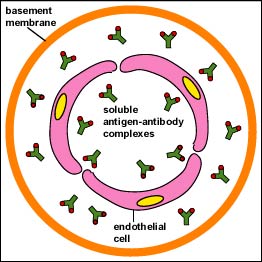
b. increased capillary
permeability. This causes swelling of local tissues (edema). If
widespread, it can contribute to decreased blood volume and
shock.
c. constriction of
bronchial airways. This leads to wheezing and difficulty in
breathing.
d. stimulation of mucous
secretion. This leads to congestion of airways.
e. stimulation of nerve
endings. This leads to itching and pain in the skin.
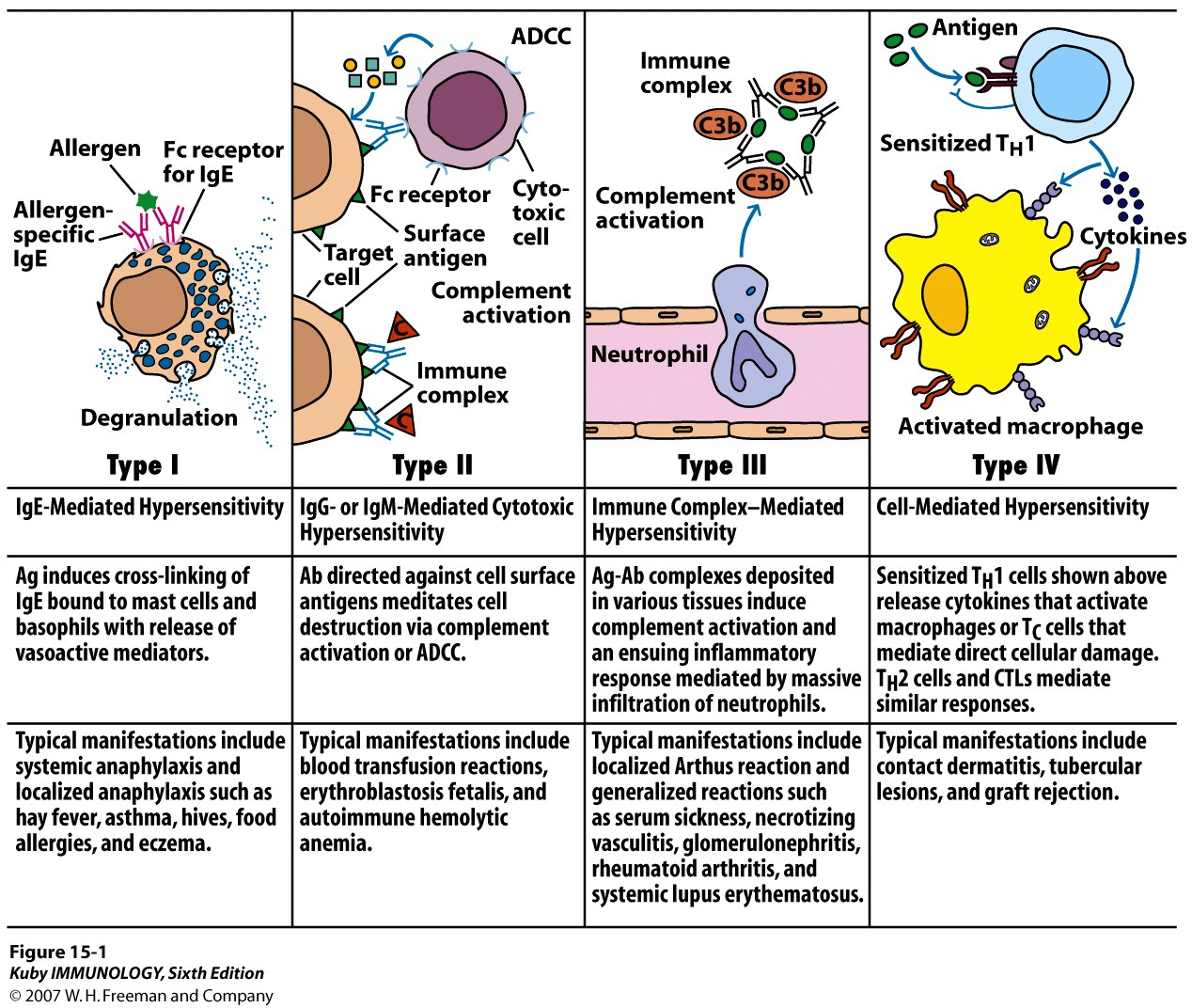
In a systemic anaphylaxis,
the allergen is usually picked up by the blood and
the reactions occur throughout the body. Examples include severe allergy to
insect stings, drugs, and antisera. With a localized anaphylaxis, the
allergen is usually found localized in the mucous
membranes or the skin. Examples include allergy to hair, pollen, dust,
dander, feathers, and food.
Type I hypersensitivity is
treated symptomatically with such agents as:
a. epinephrine.
Epinephrine relaxes smooth muscle, constricts blood vessels, and
stimulates the heart. It is used for severe systemic reactions.
b. antihistamines .
Antihistamines block the binding of histamine to histamine receptors on
target cells.
c. Nasally administered
steroids. Corticosteroids are potent antiinflammatory agents.
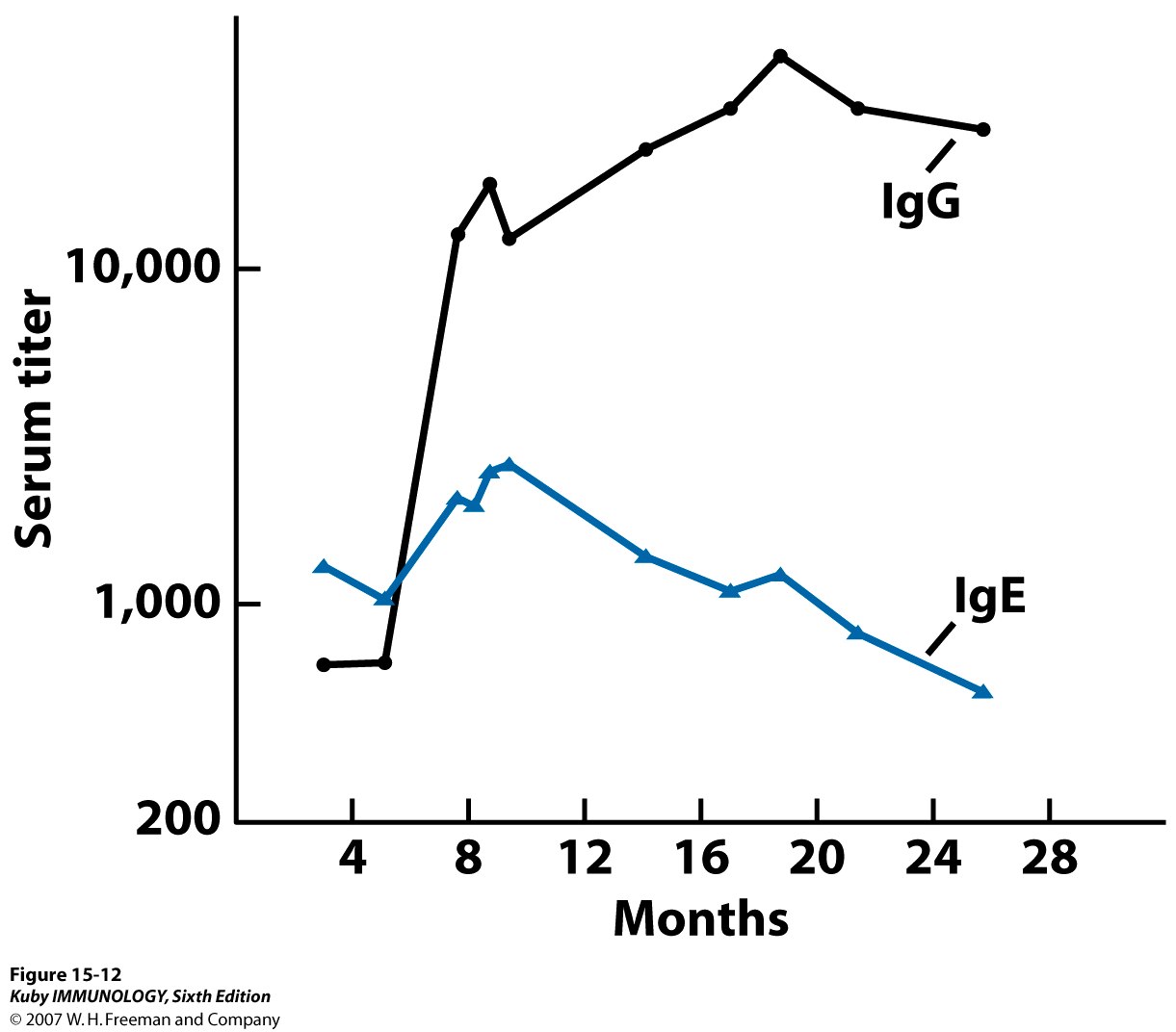
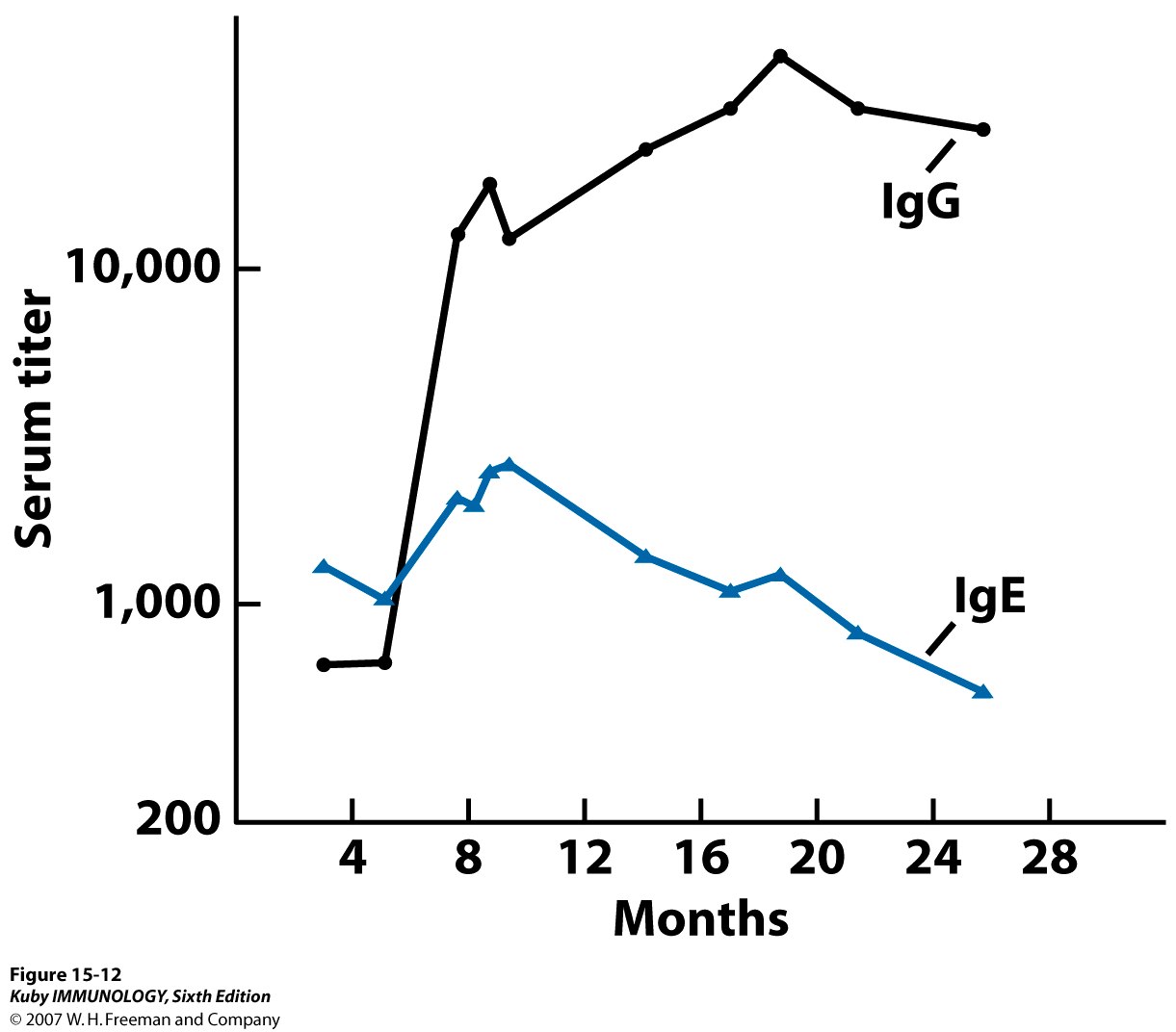
Severity may be reduced by
desensitization shots (allergy shots). It is thought that when very
dilute allergen is given by injection, it stimulates the production of IgG
IgG then act as
blocking antibodies to bind and neutralize much of the allergen in
secretions before it can bind to the deeper cell-bound IgE on the mast cells
in the connective tissue.
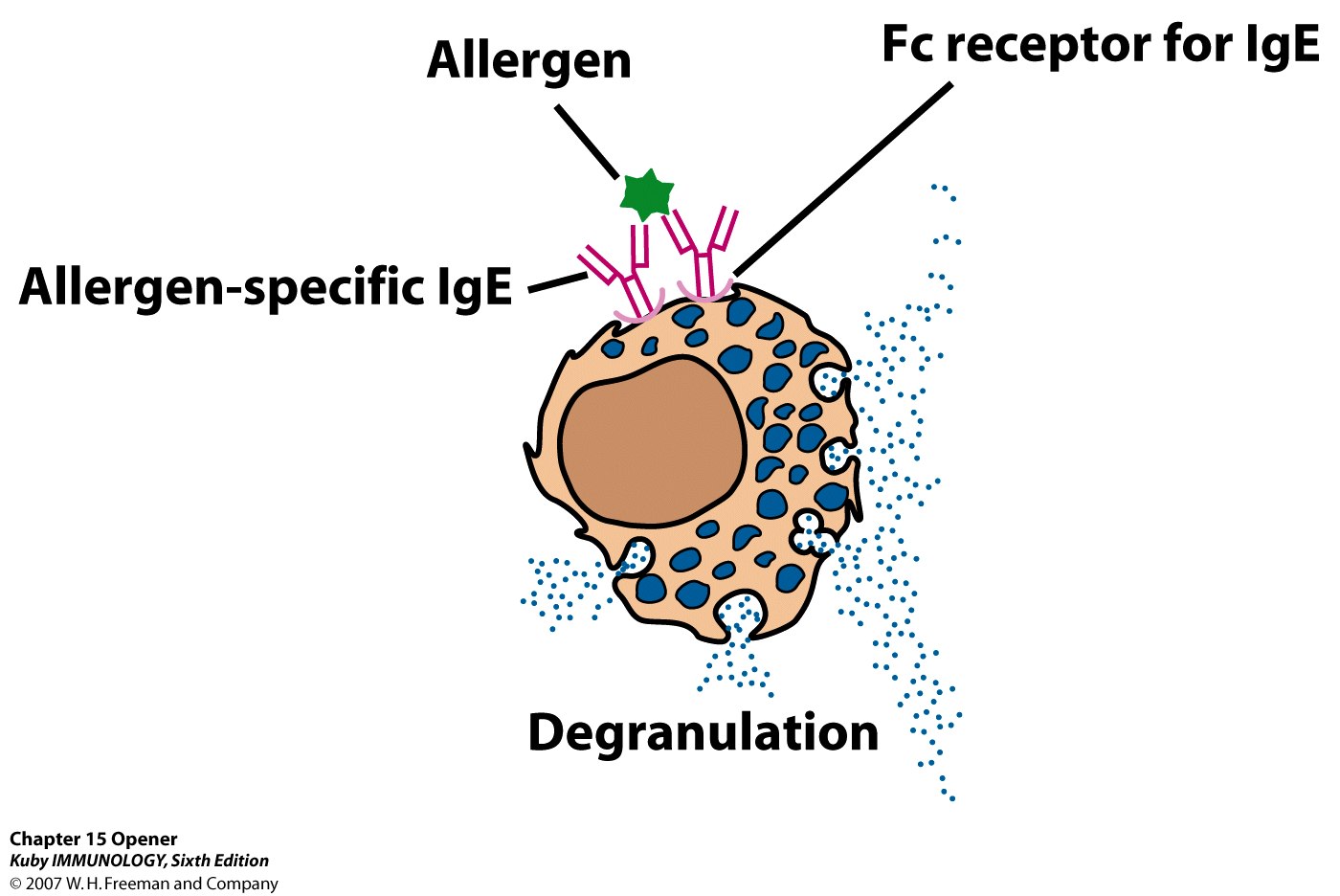
A new experimental approach to
treating and preventing Type-I hypersensitivity involves giving the person
with allergies injections of monoclonal antibodies that have
been made against the Fc portion of human IgE.
This, in turn, blocks the
attachment of the IgE to the Fc receptors on mast cells and basophils and
the subsequent release of histamine by those cells upon exposure to
allergen. In addition, the anti-IgE binds to IgE-producing B-lymphocytes
causing apoptosis.