What happens when Antibodies work against you?
Allergic Reactions
The Fc portion of IgE binds to the surface of mast cells and basophils
When the allergen cross-links the Fab portions of the mast cell-bound IgE, this triggers histamine release by the mast cell, a process called degranulation, and the synthesis of other inflammatory mediators such as arachadonic acid, leukotrienes, prostaglandins, and cytokines that contribute to inflammation (these act as chemoattractants). These agents cause the early phase of allergic reactions that appears within minutes after exposure to the antigen.
Autoimmune Disease
Mechanism: Either IgG or IgM is made against normal self antigens as a result of a failure in immune tolerance , or a foreign antigen resembling some molecule on the surface of host cells enters the body and IgG or IgM made against that antigen then cross reacts with the host cell surface. The binding of these antibodies to the surface of host cells then leads to:
a. opsonization of the host cells whereby phagocytes stick to host cells by way of IgG, and discharge their lysosomes and ;
b. activation of the classical complement pathway causing MAC lysis of the cells
c. ADCC destructionof the host cells whereby NK cells attach to the Fc portion of the antibodies. The NK cell then release pore-forming proteins called perforins and proteolytic enzymes called granzymes. Granzymes pass through the pores and activate the enzymes that lead to apoptosis of the infected cell by means of destruction of its structural cytoskeleton proteins and by chromosomal degradation.
Multiple Sclerosis
Characteristics:
Observations:
Higher levels of Ab to the myelin basic protein during flare up
Myelin BP (insulation around nerve cells)
Nerve cells become exposed
Eventual destruction of the nerve cell
What are correlations?
Disease Response
Involves T and B cells
|
B cell and T cell are autoreactive
So what is going on?
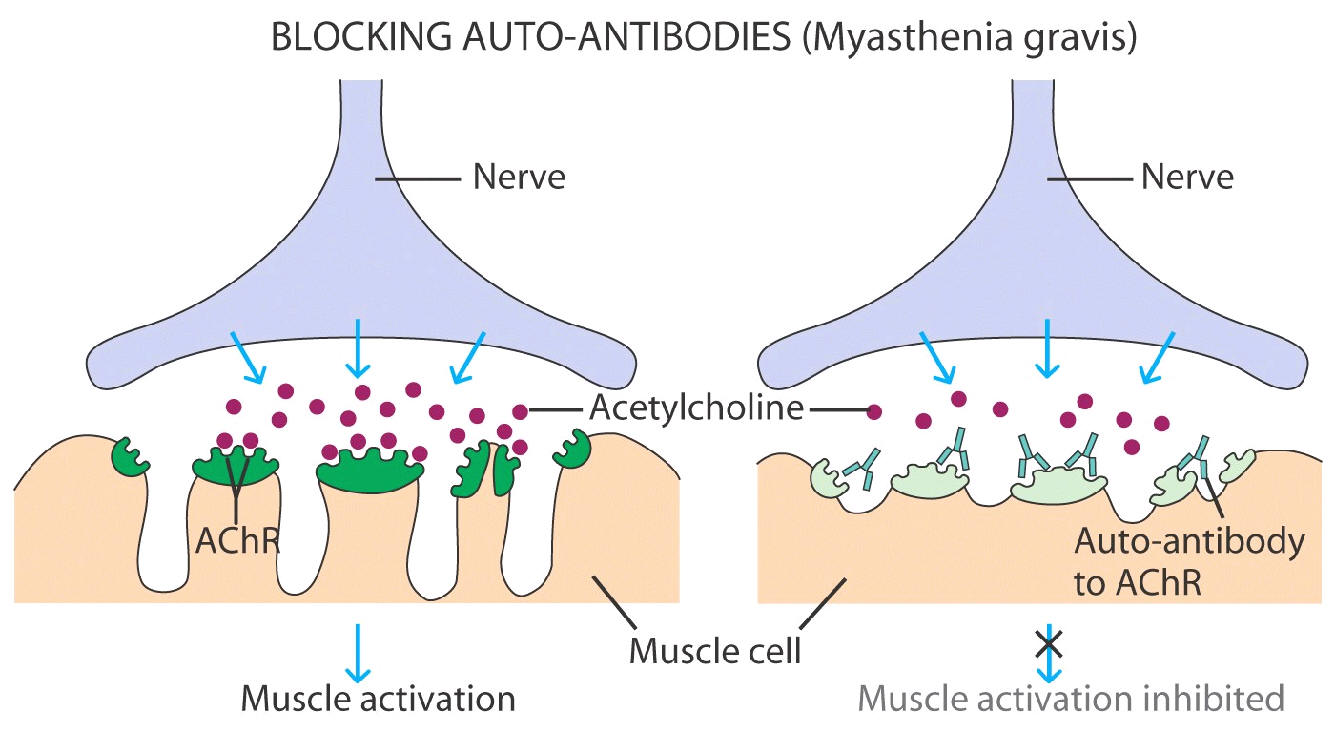
Myasthemia Gravis
Ab made to the nerve endings
Nerve endings used Acetylcholine to signal muscles
Immune Complex
Ex Rheumatoid Arthritis
Synovial fluid around joints have IgG to the cartilage (normal)
In RA there is a production of IgM that reacts with IgG (Fc) along with compliment
Tissue damage
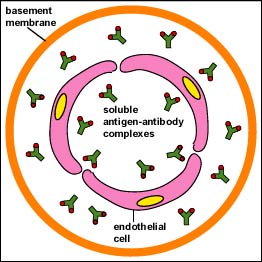
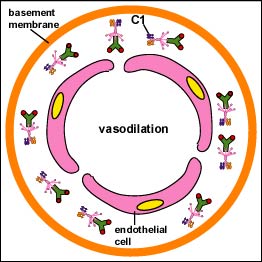
Mechanism: This is caused when soluble antigen-antibody (IgG or IgM) complexes, which are normally removed by macrophages in the spleen and liver, form in large amounts and overwhelm the body . These small complexes lodge in the capillaries, pass between the endothelial cells of blood vessels - especially those in the skin, joints, and kidneys - and become trapped on the surrounding basement membrane beneath these cells . The antigen/antibody complexes then activate the classical complement pathway . This may cause:
Lupus (10:1) (younger age 15-40)
Characteristics:
Full Blown:
Type I Diabetes
5% of diabetes
95% Type II (not AI disease as B cells are making insulin rather just non response to insulin made)
Type I = destruction of beta cells in the pancreas
Normal:
Beta cells express low levels of class I but not classII
In Type I, beta cells do express type II MHC
Beta cells are attacked self antibodies

The Mouse in Science:
Cancer Research
Mice have been used in cancer research since 1894. Initially, mice were used for same-species tumor transplantations and drug treatment studies. In 1921, inbred strains that were predisposed to getting tumors were started and disseminated among cancer researchers. Many more strains of mice were originated beginning in 1929 with the founding of the Jackson Laboratory in Bar Harbor, Maine, now the largest supplier of mice.
In 1962, the discovery of a mutant mouse with low immunity led to human tumor transplantations, a valuable breakthrough for cancer research. A further breakthrough in the late 1980s led to transgenic mice, those whose genes have been altered to produce a desired characteristic. Oncogenes, or genes that cause cancer, could then be studied in greater detail.
Life in the Laboratory.
Mice adapt well to laboratory housing and can be housed
socially or individually. Significant numbers can be housed in relatively little
space because of their small body size. They possess a surprising genetic
similarity to humans. These features, combined with a rapid rate of
reproduction, make mice the mammal of choice for fine-tuned genetic
manipulation. Mice with many different special features have been bred or
created, including some described here.

Inbred Strains.
The inbreeding of mice predisposed to developing cancer
has led to a variety of specialized strains. In 1921, Leonell Strong established
many inbred strains that frequently and spontaneously developed cancer. Serving
as a virtually unlimited source of many types of tumors, these inbred mice have
made it possible to study the growth and general characteristics of tumors.
Nude Mice.

The nude mouse is a major breakthrough for cancer research
because it allows human tumors to be studied in another animal. The nude mouse,
a hairless mutant discovered in 1962, is immunodeficient, and thus does not
reject tumor transplantations from other species. It lacks a thymus, which is
essential for the production of T-cells, lymphocytes that are essential
to the immune system. iBy transplanting an actual human tumor into a nude mouse,
the tumor can be studied in a whole animal system.
Before discovery of the nude mouse, human tumors were grafted and grown in immune-privileged sites, such as the anterior chamber of the eye, the brain and the cheek pouch. These locations are inconvenient, and the tumors are eventually rejected. The recessive nu gene, which is responsible for the lack of a thymus in nude mice, has since been introduced into many types of inbred strains of mice with other immunodeficiencies.
SCID Mice.

In 1983, mice with severe combined immune deficiency (SCID)
were discovered. SCID mice are even more immunodeficient than nude mice. Tumors
from other species are easily transplanted into SCID mice and will grow without
being rejected. For certain specific tumors, SCID mice show improved
transplantability over nude mice. In addition, SCID mice are ideal for the
growth of hybridomas in vivo to produce a continuous supply of
antibody (Ab). Sometimes referred to as a reagent, Ab is necessary for a wide
range of diagnostic, clinical and experimental procedures.
Transgenic Mice.
In the late 1980s the methodology for engineering
transgenic mice made it possible to create mice to address specific questions
and problems. Transgenic mice result from genetically altered embryos: a gene or
combination of genes is microinjected into developing oocytes. The genetic
alteration affects the germ plasm, and subsequently can be transmitted to
progeny. Through selective breeding, it then is possible to maintain a strain of
mice consisting of individuals with particular traits of interest.
A specific trait, such as a predisposition to develop a particular type of tumor, can be introduced into a mouse strain by injecting into the embryo an oncogene, a gene that causes cancer. Transgenic mice permit the study of cancer in specific tissues, including initial tumor development.
Uses.
The purpose of cancer research is to understand tumor
initiation and growth. This information helps researchers develop treatments,
and eventually cures, for cancer.
| |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
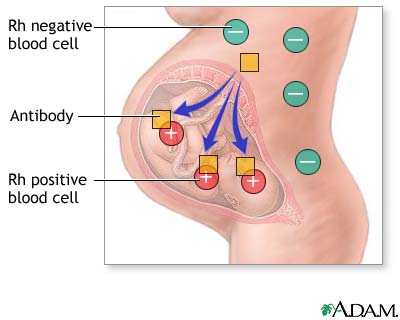
Rh incompatibility occurs when the mother's blood type is Rh negative and her fetus's blood type is Rh positive. An alternative name is Rh disease. Rh is an abbreviation for Rhesus.
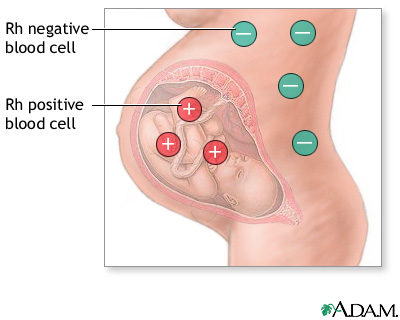
Everyone is born with a certain blood type that is either Rh positive or Rh negative. Rh-positive blood is more common than Rh-negative blood. About 85% of Caucasians are Rh positive, while the percentage is even higher for African-Americans, Asians, and American Indians. If you are Rh positive, or if both you and the baby's father are Rh negative, there is no reason to worry about Rh incompatibility. However, if you are Rh negative and the baby's father is Rh positive, then your baby may inherit the father's blood type, creating incompatibility between you and the fetus.
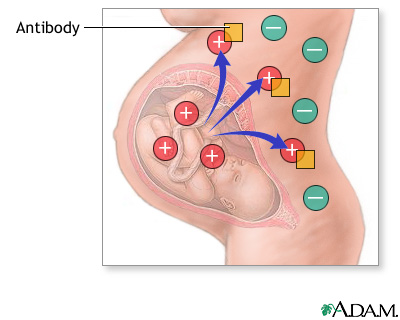
With Rh incompatibility, if some of the fetal blood gets into your blood stream, your body will produce antibodies. These antibodies could pass back through the placenta and harm the developing baby's red blood cells, causing very mild to very serious anemia in the fetus. Your first baby is usually safe, because fetal and maternal blood usually do not mix until delivery. If your second baby is also Rh positive, there's a risk that your antibodies will attack her blood cells and cause problems.
| Organ transplants and rejection | |
|
All your body cells have markers on their surface that signal to your lymphocytes and make sure that they are not attacked by your own immune system. They are called the tissue-type markers. Before a patient receives a donated organ, such as a kidney, great care is taken to match the donor's and recipient's tissues-type markers so that they are as similar as possible. They are usually quite close in family members and only ever a perfect match in genetically identical twins. Even a slight mis-match could mean that the organ was attacked by the recipient's immune system and rejected. To try and prevent transplant rejection, recipients will also take medicines to reduce the efficiency of their immune system. These medicines are called immunosuppressants. They reduce the chances of the donated organ being attacked by the recipient's immune system but they also increase the likelihood of them catching infectious diseases. A balance needs to be maintained where there immune system does not reject the transplant while the recipient is not harmed by dangerous infections. |
|