Memory
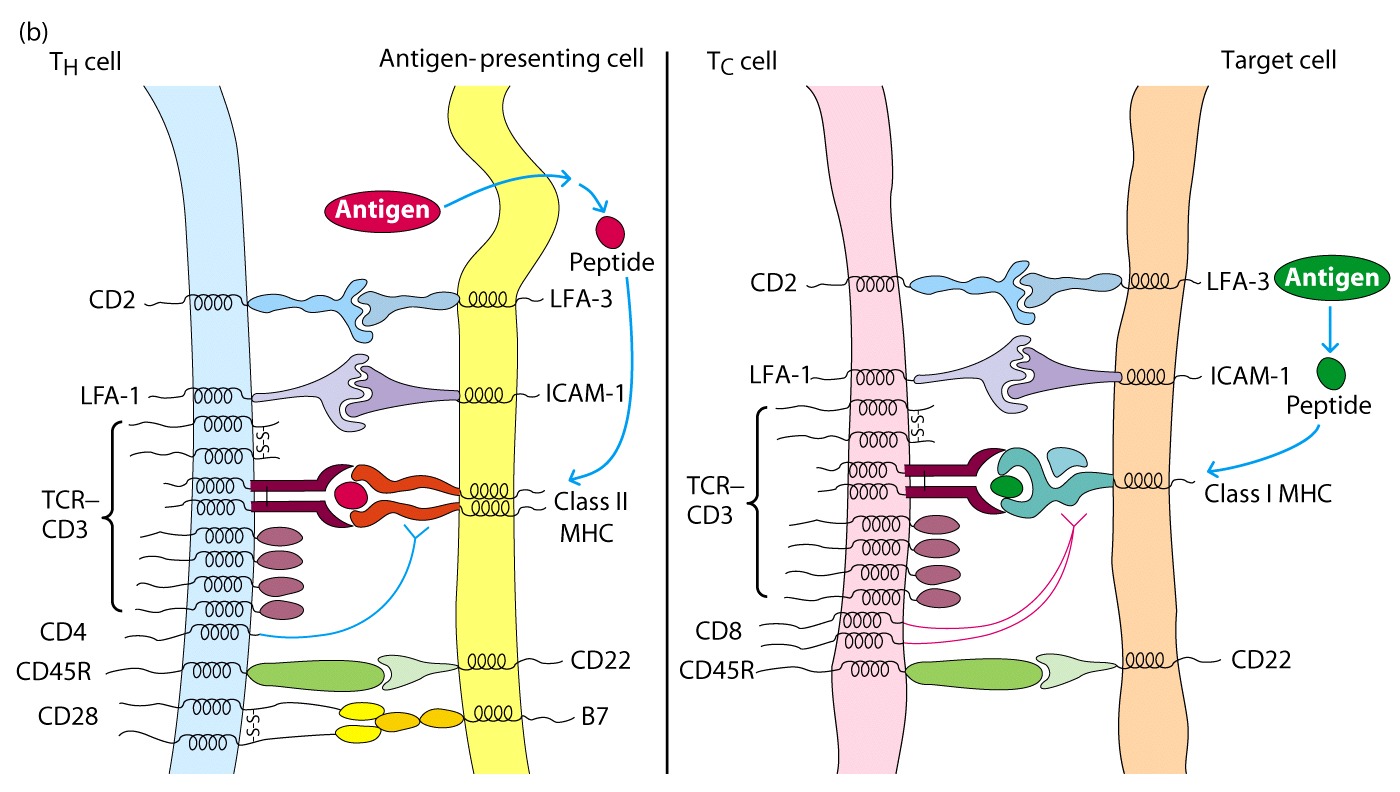
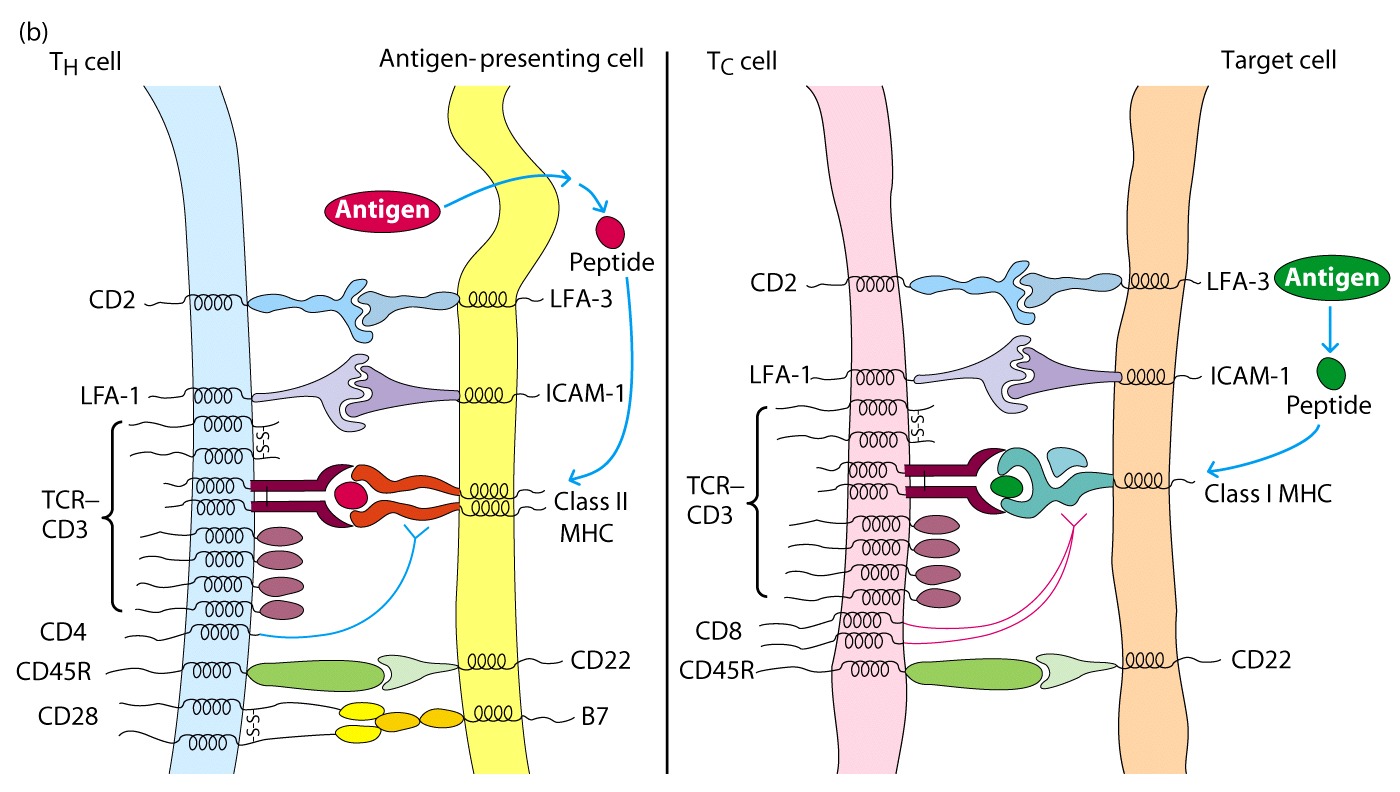
These molecules do not
interact with the MHC, but bind to other ligands on APC and strengthen
adhesion
CD28 on CD4+ T cells
interacts with B7 on APC and this interaction serves as a costimulatory signal
for T cell activation.
Memory
If
you have a naive T cell ( never been activated), then it will have to have all
the adhesion molecules present to be activate
If
the cell is a T memory cell (previously activated), then it is easier to
activate and doesn't require all the adhesion molecules to be present
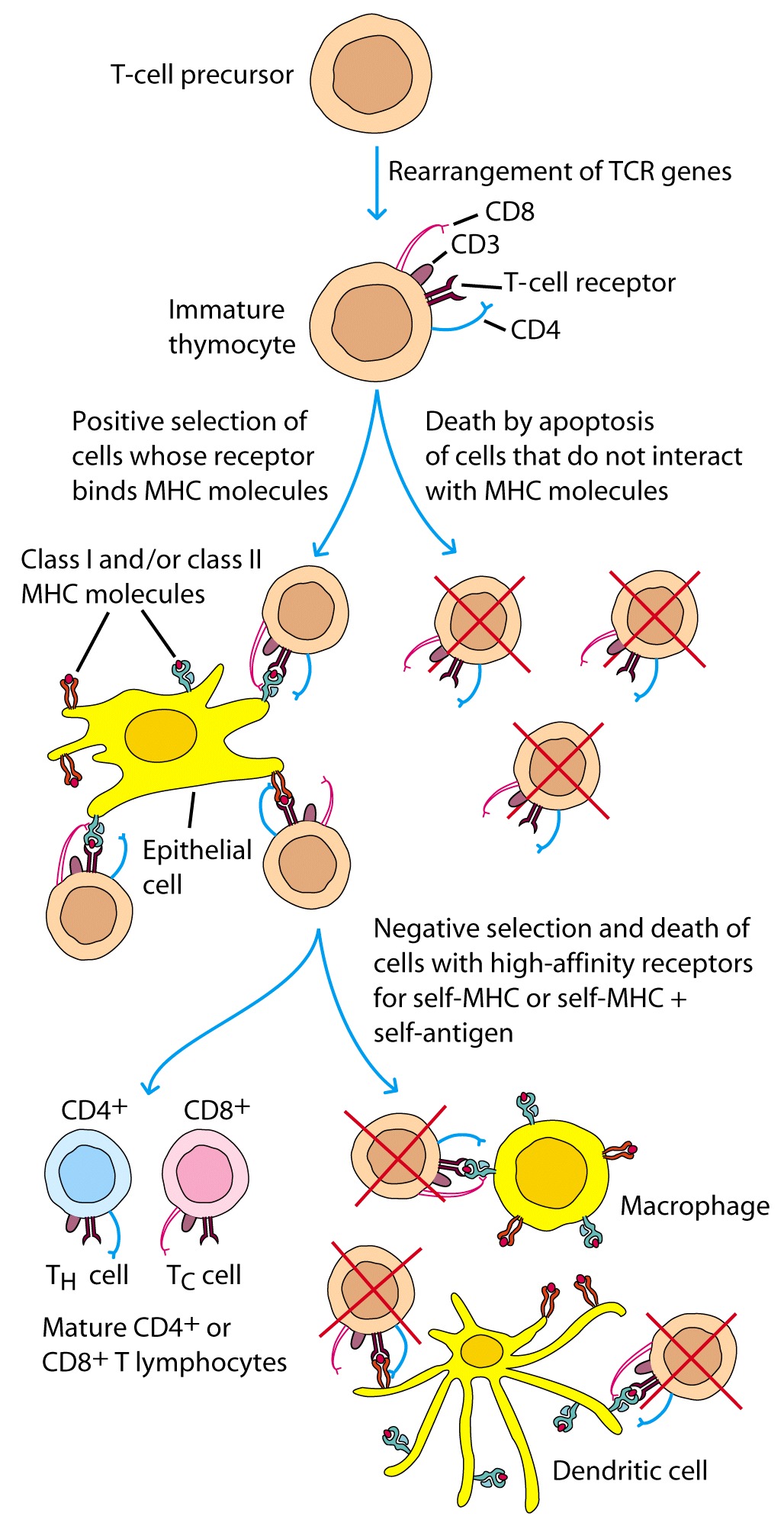
T Cell Maturation
When is this occurring?
Self vs non-self determination
Taking a closer look at what is going on in the thymus:
Early marker seen in pre T cells is Thy 1
This is the only marker that tell us that this will in fact be a T cell. It is the precursor to CD4/CD8
Note:
The γ, δ cell is primarily found in skin and may play a role in injury prevention by binding to bacteria
They never express CD4 or CD8 and they see intact proteins like Ab. They don't need to be presented by APC or recognize self like Tc cells
They may express another gene that stops their destruction
Next Step
Good figure from text
Concept:
Tolerant to self because the weak interaction doesn't trigger a response
Therefore
![]() TH
= CD4+ CD8-
TH
= CD4+ CD8-
![]() Tolerant
to self
Tolerant
to self
Tc = CD4- CD8+
Clonal Anergy Ensues If a Co-Stimulatory Signal Is Absent
TH cell recognition of an antigenic peptide/MHC complex sometimes results in a state of nonresponsiveness called clonal anergy, marked by the inability of cells to proliferate in response to a peptide MHC complex
Whether clonal expansion or clonal anergy ensues is determined by the presence or absence of a co-stimulatory signal such as that produced by the interaction of CD28 and B7 on APC's
Bringing it all together
cell development occurs in the thymus (clinical, DiGeorge, nude mice). T cell precursors however arrive to the thymus from the Bone Marrow. The stages of T cell development are identified by the expression of specific cell surface markers, such as TCR (T Cell Receptor), CD3 (which serves as the signal transduction component of TCR), and CD4/CD8. Direct cell to cell interaction between these cells and thymic cells induces their proliferation and also differentiation. Pre-T cells do not express any of the above mentioned T cell markers. At this stage they are referred to as Double Negative cells (because they are CD4 and CD8 negative). At this point the beta-chain of TCR undergoes rearrangement. The successful rearrangement of this chain serves as a signal for these cells to undergo further proliferation. During this time, both CD4 and CD8 start to be expressed, thus these cells are referred to as Double Positive cells. It is only at this point that the alpha-chain of the TCR undergoes rearrangement. At this stage these cells undergo the processes of Positive and Negative selection.
Positive selection:
Since TCR's recognize antigen only in the context of MHC's, T cells must be
tuned to recognize host MHC first. During positive selection Double-Positive T
cells that can recognize self MHC's are selected for proliferation, and those
T cells that do not recognize self MHC die via Apoptosis. Positive selection
also assures that the right TCR selection will go with the appropriate CD4 or
CD8. For example, TCR's specific for MHC II need to retain CD4, and lose CD8.
If the reverse occurs, they will die via apoptosis. The same is true for the T
cells that are specific for MHC I, which need to retain CD8, and lose CD4
(Reminder: CD4+ Th cells recognize MHCII,
and CD8+ Tc cells recognize MHC I)
Negative selection:
At this point, those T cells that are strongly activated by self MHC plus self
peptides need to be eliminated in the thymus. If they escape this elimination,
they may subsequently react against self antigens, and cause Autoimmune
disease.
In summary, Positive selection selects for those T cells that react with
MHC: self antigen. Negative selection eliminates those that react strongly
with MHC: self antigen. Thus, successful T cell differentiation selects for
MHC restricted TCR's with low affinity for self antigens.
Cells that fall outside this
range, primarily die via apoptosis. The rationale here is that a T cell that
binds weakly to self MHC/self Antigen will not be activated but will be
activated by a stronger binding to self MHC/ foreign Antigen
complex..
T helper cell
A T helper cell, is a T cell (a type of white blood cell) which has on its surface antigen receptors that can bind to fragments of antigens displayed by the Class II MHC molecules found on professional antigen-presenting cells (APCs).
Once bound to an antigen, the TH cell proliferates and differentiates into activated TH cells and memory TH cells.
Most TH cells have present on the cell surface the protein CD4, which is attracted to portions of the Class II MHC molecule. This affinity keeps the TH cell and the target cell bound closely together during antigen-specific activation. TH cells with CD4 surface protein are called CD4+ T cells. The decrease in number of CD4+ T cells is the primary mechanism by which HIV causes AIDS.
|
|
|
|
||
|
|
|||
|
At least three forms of T-helper-cells (Th) may be distinguished on the basis of their cytokine repertoire: Th0, Th1, Th2 |
|
|||
|
|
Click here for description of cell types |
|
|
|
|
|
|
|||
|
Th1-cells primarily produce interferon gamma (IFN-gamma), interleukin (IL)-2, lymphotoxin (LT)a and granulocyte-macrophage colony-stimulating factor (GM-CSF); they are particularly important in cell-mediated immune reactions. Th2-cells primarily produce IL-3, -4, -5, -6, -10 and -13; they are particularly important in antibody-mediated immune reactions. Dendritic cells (DC), specialized in presentation of antigen to Th, appear to decide whether Th1- or Th2-type cells are activated. Hence, DC1 secrete IL-12, which differentiate Th0 to Th1, and DC2, perhaps through production of an unknown cytokine (which is not IL-4), favors differentiation to Th2 cells. |
|
|||
There are two distinct kinds:
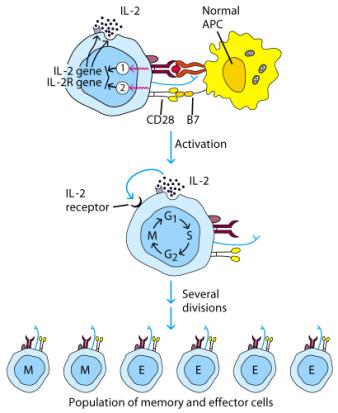
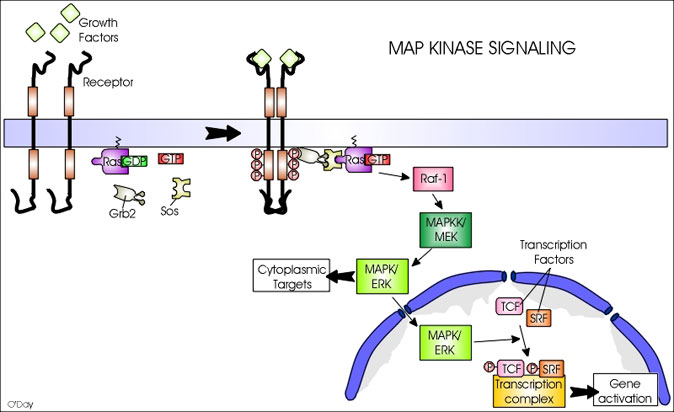
T Cell Proliferation
The
RAS signaling pathway is triggered by activation of the RAS gene.
Getting rid of unwanted cells
Apoptosis
Q. What is the difference between apoptosis and necrosis?
Pro-life vs Pro-death
Akt is constitutively on in Her2 neu (human breast cancer)
Q. Chemo - focused on what aspect of these signaling pathways?